Medical experts share the 17 most common medication mistakes that you should avoid to make sure you don't get sick.
Medication mistakes to avoid
It’s not uncommon to make a mistake when you take your medication. This is especially true if you take more than one medication and also have several health conditions. An incorrect dose, the wrong drug, or misunderstanding the prescription label can contribute to medication mistakes at home.
Although you may shrug this off as a mishap, medication errors can actually injure people and land them in the emergency room.
1. Not understanding medication dangers

The number of home medication errors that resulted in calls to Poison Control doubled over a 13-year study period, according to a 2017 study in Clinical Toxicology, and that’s only the mistakes that were phoned in. Luckily, most of those mistakes weren’t life-threatening, but they can be: One-third of the medication errors in the study resulted in hospitalization. The first step to avoiding these mistakes is awareness of how serious they can be. And be familiar with the over-the-counter (OTC) medications you’re using, could be used in the wrong way too.
2. Taking too high a dose

Even too much Tylenol can cause serious liver damage, according to the U.S. Food and Drug Administration (FDA). (These are the hidden dangers of OTC meds.) “If you take a dose that’s too high, you may have an increased chance of side effects—for example, increased drowsiness from pain medication or bleeding from too much anticoagulant, such as Warfarin [Coumadin]—due to having too much of the medication in your body,” says Barbara Young, PharmD, MHA, editor of consumer medical information for the American Society of Heath-System Pharmacists
3. Taking meds too often

In a 2018 study, published in Pharmacoepidemiology Drug & Safety, researchers at Boston University found that 15 percent of those who use NSAIDs (non-steroidal anti-inflammatory drugs) like Advil or Aleve exceed the recommended dose in a one-week period, which can lead to serious side effects like intestinal bleeding and even heart attacks. For prescription meds, it’s important to stick to the dosing times to avoid overtaxing your body. “Several mechanisms to remove the drug from the body usually involve the liver or kidneys, or both, so if you have problems with either, your doctor may tell you to take a lower dose or take your medication less frequently,” Young says.
4. Taking too low a dose or too infrequently

If you don’t take your meds as directed, you may be putting your health at risk. For example, one of the things you can do to prevent deep vein thrombosis (DVT), a deadly blood clot in your leg, is to keep up your proper dosing of blood thinner, if that’s been prescribed to you. “The body metabolizes a drug at a certain predicted rate, so taking them on the prescribed schedule is important to maintain this consistent level,” Young says. “Think of a bucket with a small hole in the bottom—if you want to maintain a certain level of water you must add a certain amount, or dose, at certain intervals.” If you add too little or wait too long, the water level will fall too low.
5. Taking meds with—or without—food

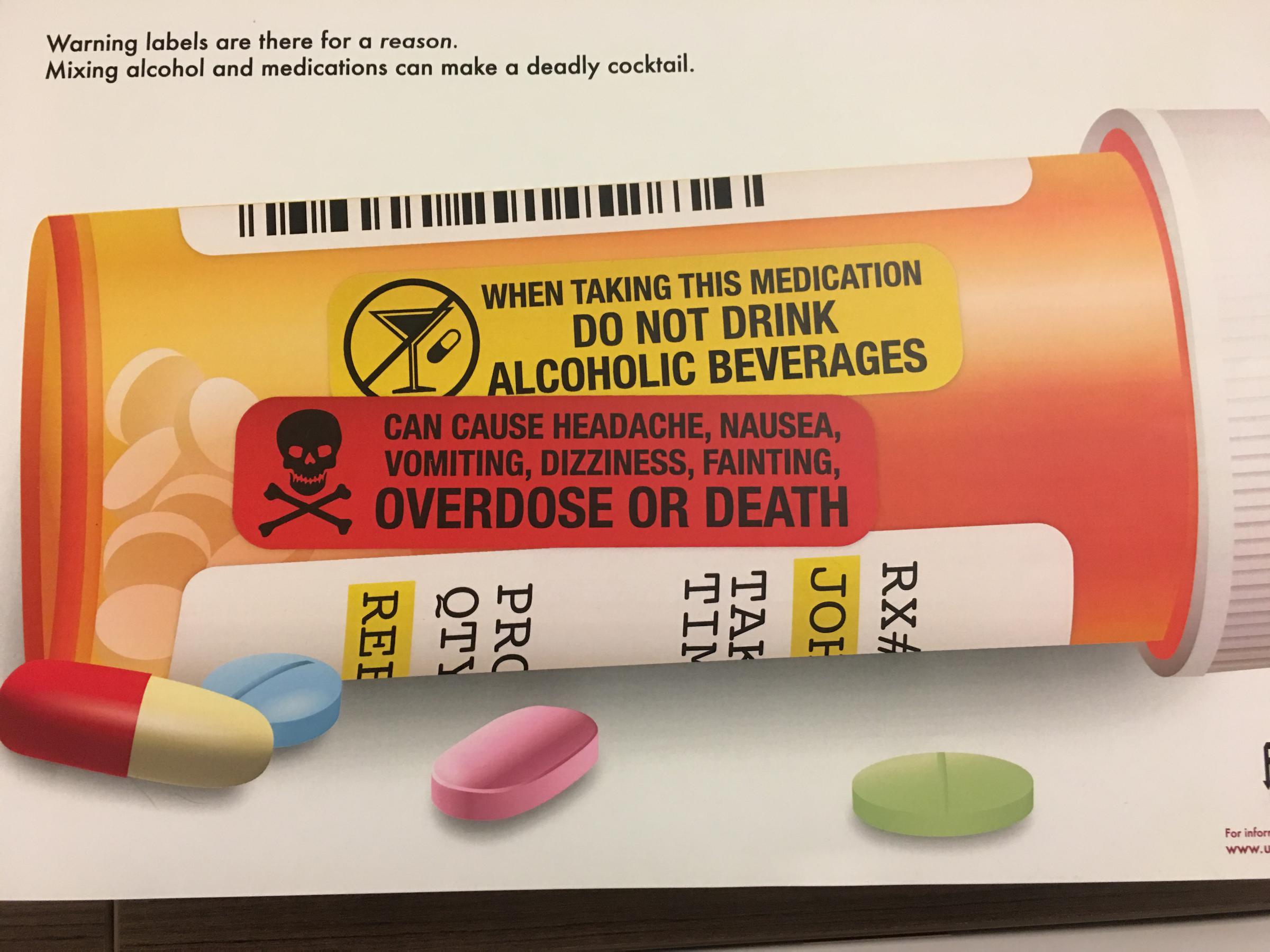
The directions on the prescriptions are not just suggestions. “For some medications, food, or certain types of food, will affect how the drug is absorbed from the stomach into the body,” Young says. Some may be absorbed too slowly or not as fully with food, such as the osteoporosis medication, Fosamax, or the thyroid drug Synthroid. So, take them on an empty stomach or within a certain period of time before you eat again. “On the other hand, some medications may irritate the stomach, such as NSAIDs including ibuprofen, and are best taken with food to minimize any irritation,” Young says. Read the label or ask your pharmacist if you should take your meds with or without food. Plus, there are many medications that you should not mix with alcohol.
6. Not avoiding specific foods

Even if you take your meds with a meal, you may not realize you should avoid some foods. “Certain antibiotics should not be taken with calcium-containing food or [calcium-containing] OTC drugs, which will affect how they are absorbed by the body,” says Dave Walker, RPh, medical advisory board member, MedShadow Foundation. “Calcium can actually inactivate antibiotics, including tetracycline and doxycycline” adds Walker. Plus, “the metabolism of several medications, including statins, is affected by the enzymes in grapefruit juice,” Walker says. Ask your pharmacist if there are any food interactions to avoid with your meds.
7. Mixing meds inappropriately

Your meds could also be making you sick. It could be because you’re inadvertently counteracting or doubling up on meds—and this includes OTC drugs, vitamins, and herbal supplements. “The interaction can increase or decrease the effectiveness of the medicines, cause unexpected side effects, or increase the risk of known side effects,” says Michael J. Gaunt, PharmD, medication safety analyst, editor, ISMP Medication Safety Alert! Community/Ambulatory Care Edition at the Institute for Safe Medication Practices (ISMP). For example, some meds should not be taken at the same time as antacids because the absorption may be changed by the reduction in stomach acid, Young says.
8. Not getting a medication schedule from your doctor

It’s important to make sure your doctor or pharmacist knows all of the prescription and over-the-counter medications, supplements, and vitamins you take in order to come up with an approved list for when to take each of them. “If you take a number of medications, consult with your pharmacist to find the best schedule for you to take them,” Young says. “If you group your medications to take at similar times, it will improve your chances of taking your medications consistently and on time.” Just make sure your healthcare provider is on board with the plan.
9. Not understanding your prescription label

It’s easy to get confused when it comes to reading prescription labels, and science agrees too. Previous research from Northwestern has shown that prescription labels are notoriously hard to understand due to awkward wording. The researchers found that among 395 English-speaking adults waiting to see their providers, patients with lower literacy levels and those who were prescribed more meds were less likely to understand the prescription labels. However, even among patients who were able to understand the labels, only a small portion could interpret how to take the pills correctly. Make sure you confirm everything with the pharmacist before taking your meds.
10. Not knowing what your medication is for

You should be aware of what each drug is for when you start taking it. “Having an understanding of the condition or disease that the medication is being used to treat will help you also understand the importance of taking it,” Young says. “Often medications may be used to treat more than one condition, so know why you are taking the medication, especially when you talk to other doctors or healthcare professionals.”
11. Not knowing the names of your meds

Avoid confusion and reduce the likelihood of making a mistake by knowing the names of the drugs you take. “Studies show that patients who know the names of their medications have better adherence to their medication regimen and are less likely to mix up their medications or take the wrong one,” Walker says. “Knowing both the brand name and generic name of a medication is especially helpful since the prescriber may be using the brand name to prescribe, while the pharmacy would usually dispense the generic name.”
12. Not checking the label
Pharmacists can sometimes make mistakes. “We at ISMP regularly receive reports of pharmacies giving a correctly filled prescription to the wrong customer,” says Gaunt. In a 2012 study, published in the Journal of the American Pharmacists Association and conducted by ISMP, they found that this error happens about once for every 1,000 prescriptions filled. Taking the wrong drug may cause an adverse reaction or leave your condition untreated, so check that the label is correct before you leave the pharmacy. In addition, make sure the pills look the same each time you refill them, Gaunt says—if they don’t, you could have the wrong meds.
13. Not taking your meds correctly

It may seem obvious at first glance, but you’d be surprised at how easy it is to mess this up. Common mistakes include mixing up eye and ear drops, chewing non-chewables, using silverware to measure teaspoons, and cutting up pills. Understanding the right way to take your meds “will assure that you get the correct dose or appropriate amount of medication for each dose, which is especially important for medications that have a narrow range for dosing,” Young says. “Knowing which products may be chewed or crushed is also important as some medications will be absorbed too fast or in too high a dose if crushed or chewed.” A good rule to follow: When you pick up your meds, confirm with your pharmacist exactly how to take it.
14. Stopping your meds too soon

You feel better, so you can stop your meds, right? Wrong. “Stopping a medication abruptly can lead to severe consequences,” Walker says. Your blood pressure or blood sugar levels could spike if meds to manage them are stopped. “Some medications may have adverse effects when stopped suddenly, including SSRIs such as Prozac, which takes time to build in the system to become effective,” he says. With antibiotics, “although you may feel better after a few days, all of the bacterial infection causing the symptoms is probably not yet eradicated until the full course of treatment is completed.” To avoid getting sick again, complete the full course.
15. Taking other people’s meds

Your friend swears by her prescription drug, but that doesn’t mean you should take it if she offers. “Well-meaning individuals may think to share their prescription medicines with others to help treat their symptoms,” Gaunt says. “However, a medicine’s effect depends upon the individual’s medical conditions and their tolerance to the medicine. Sharing of meds, such as powerful opioids [pain medicines], has resulted in patient harm, including death.” Even if you feel your symptoms aren’t being adequately handled by your doctor, don’t use someone else’s meds—instead, get a second opinion.
16. Taking too many meds

According to the Centers for Disease Control and Prevention, 29 percent of American adults take five or more meds. “Every time you add another medication you can almost count on increasing the chance of side effects, adverse drug reactions, and drug-drug interactions,” Walker says. Sometimes, you’re prescribed more drugs to control the side effects of other drugs. For example, “ADHD medications can change sleep patterns that need to be balanced with other medications; or opioids cause sedation which sometimes leads to stimulants being prescribed,” Walker says. “It’s paramount that you speak to your prescriber and pharmacist to fully understand the potential risks associated with taking multiple medicines.”
17. Storing and disposing of meds incorrectly

Drugs, including OTC meds, need to be stored accordingly to maintain their effectiveness. “Medications may require a certain temperature range, protection from light, or protection from humidity to maintain the product integrity so the medication won’t physically change or lose potency,” Young says. That means not storing them in the bathroom where temperature and humidity changes. In addition, you should dispose of unused meds according to the FDA’s guidelines. “Proper medication disposal is critical to reduce harm from accidental exposure and intentional misuse by others for whom the medicine was not prescribed,” Walker says.
The AgilityRx Card is easy to use Simply present the AgilityRx Discount Card along with your health insurance card and ask your pharmacist to process your prescription with the plan that provides you with the lowest cost.